Innovative partnership epitomizes transformative CAMLS training center
The USF Health-Symbionix team is creating the first simulation product on the market for laparoscopic hysterectomy
USF Health physicians are an integral part of an international team developing the world’s first laparoscopic hysterectomy simulation module — an academic entrepreneurial partnership that may help change how future obstetrician-gynecologists learn.
Dr. Stuart Hart and Dr. Larry Glazerman, faculty members in the USF Health Department of Obstetrics and Gynecology, last month visited Israel to work with engineers from Simbionix™ on the project. The partnership is funded by a two-year, $700,000 grant from the U.S.-Israeli Binational Industrial Research and Development (BIRD) Foundation. Dr. Hart and Dr. Glazerman are principal investigators for the grant, which supports the creation of a laparoscopic hysterectomy simulation module for training GYN surgeons in advanced minimally-invasive surgery techniques.
“Our goal is to make the learning experience as close as possible to the real operation,” said Dr. Hart, assistant professor in the USF Health Division of Urogynecology and Pelvic Reconstructive Surgery. “We’re part of a team designing technology that will help transform the future of health care by making surgery safer and more efficient.”

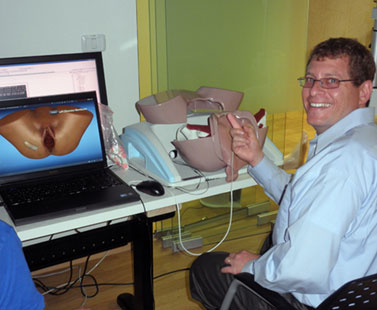
USF Health’s Dr. Stuart Hart, left, and Dr. Larry Glazerman, experts in minimally-invasive gynecological surgery, visited the Simbionix Research and Development Center in Tel Aviv, Israel, to work on the simulation prototype with engineers.
Symbionix and USF Health plan to roll out the prototype laparoscopic hysterectomy simulation module in November at the American Association of Gynecologic Laparoscopists 40th Global Congress of Minimally Invasive Surgery in Hollywood, FL. Those attending will have to opportunity to try out the prototype.
When the project is finalized this spring, the USF Health Center for Advanced Medical Learning and Simulation (CAMLS) will be the beta test site for the simulation module, allowing ob-gyn faculty, residents and practicing physicians to provide feedback on the new Simbionix product.
USF Health will also work closely with the American College of Obstetricians and Gynecologists (ACOG) to scientifically validate the module’s educational content so that it may be integrated into training programs in the future.
The training module is designed to run on the Symbionix
LAP Mentor simulator.
USF Health’s collaboration with Simbionix is the type of innovative project that will be encouraged by the Tampa Bay Research and Innovation Center (TBRIC), a center within CAMLS dedicated to advanced medically related engineering research and development, medical modeling and simulation, human factors analysis and medical device development, said Dr. Hart, the center’s TBRIC medical director.
“Partnering with a global company like Simbionix, obtaining the BIRD Foundation grant, and working with a national specialty society like ACOG to validate the performance metrics of this new simulation product epitomizes what CAMLS is all about,” said Deborah Sutherland, PhD, associate vice president of USF Health and CEO of CAMLS. “We anticipate many similar projects once CAMLS opens in Spring 2012.”
During the visit to the Simbionix Research and Development Center in Tel Aviv, Israel, Aug.21 to 24, Dr. Hart and Dr. Glazerman worked directly with the development team to modify and refine the simulation module. This included performing multiple hysterectomy procedures using the prototype module and giving their input about the anatomic and surgical procedural improvements needed to create a realistic surgical simulation training experience. They also helped define the educational and training content for the hysterectomy module.

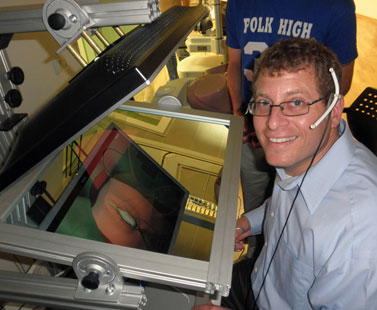
Dr. Glazerman moves the instruments while Simbionix product manager
Maya Bloch brings up an anatomical image on the monitor. Sophia Slepnev
takes notes in the background.
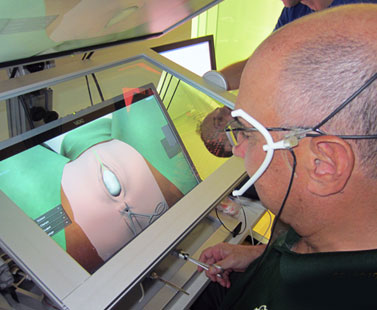
As in real life, the simulated laparoscopic operation is performed entirely by movements of the instruments and observation on a video screen. The surgeons operate while observing the movement of the instruments in a three-dimensional anatomical environment, created by the endoscopic camera on a monitor. Robots simulate the ports into which the laparoscopic instruments are inserted, allowing accurate spacial tracking in this three-dimensional surgical simulation.
The Israel trip followed a full year of preliminary work, which included videoconferences with the engineering team to design the prototype. Simbionix product managers Sophia Slepnev and Maya Bloch visited USF Health this spring, observing and videotaping ob-gyn faculty and residents performing laparoscopic hysterectomies in the operating room. This helped the engineers in critically dissecting the entire procedure down to each step – including hand motions, positioning of instruments and visual landmarks used by the surgeon in navigating the peritoneal anatomy.
The Simbionix-USF Health team collaborated to make the simulated surgery not only visually accurate but feel life-like from start to finish. The module integrates haptic technology, which facilitates the sense of touch physicians experience when inserting instruments, grasping tissue, cutting, suturing or performing other procedures. So for instance, pushing a surgical instrument into the “virtual” uterus would yield the same initial give and then tension of uterine tissue.
“The collaboration between Simbionix and USF Health will ensure that the module incorporates all clinically relevant aspects of the procedure, including complications and objective performance analysis,” said William Lewandowski, vice president for U.S. business development at Simbionix USA Corporation.
Hysterectomy, removal of the uterus, is the second most common major operation among women in the United States. Approximately 600,000 hysterectomies are performed yearly in the United States at a cost of nearly $5 billion, according to the Centers for Disease Control and Prevention.
Dr. Hart, above, and Dr. Glazerman, below, try out the true-to-life, interactive training module using the simulator’s 3-D head tracking system.
While studies indicate that many hysterectomies could safely and successfully be performed using laparoscopic techniques, the majority of these surgeries are still done by making a large abdominal incision. Despite laparoscopic surgery’s advantages in appropriately selected patients — less postsurgical pain and complications, quicker recovery times and smaller scars — obstetrics and gynecology has lagged behind other fields in adopting this minimally-invasive procedure, said Dr. Glazerman, associate professor and director of minimally invasive gynecologic surgery at USF Health.
There is a great need for scientifically-validated advanced simulation training that will help practicing ob-gyns to transfer surgical skills used in “open” abdominal hysterectomies to the endoscopic camera and video monitor, as well as train residents in the latest techniques for laparoscopic hysterectomy, Dr. Glazerman said.
“The end product of our project will be a huge benefit in helping ob-gyns adopt minimally invasive hysterectomy in a way that improves patient outcomes.”
– Story by Anne DeLotto Baier, USF Health Communications

