“Pharmacists should move from behind the counter and start serving the public by providing care instead of pills only. There is no future in the mere act of dispensing. That activity can and will be taken over by the internet, machines, and/or hardly trained technicians. The fact that pharmacists have an academic training and act as health care professionals puts a burden upon them to better serve the community than they currently do.”
( Pharmaceutical care, European developments in concepts, implementation, and research: a review.1,p.x)
This was a statement taken from the epilogue of an article published in 2004-05. Fifteen years later, we still have not developed a ubiquitous presence of pharmacist clinicians in alternative clinical environments. Many healthcare practitioners mainly associate pharmacists only as dispensers of medications. The general public is a bit more savvy, as they identify their pharmacists as medication experts that can make the time to explain how the medications are hopefully treating their medical condition, possible adverse effects, and methods to optimize the effectiveness of their medications.
However, many people in the public, including some health providers, still do not view the pharmacist clinician as a member of their total healthcare team. As outcome-driven healthcare continues to quickly evolve in our health systems across the country, profound shifts in the perceptions of the most effective roles of the various clinical professionals must begin to occur. Patients, providers, payers, and insurers must remove their traditional, decades-old view of siloed healthcare. They must all begin to truly expect, even demand, patient-centered care. As in, the patient is truly the Center of attention, and all other health providers are encircled around the patient to provide their individual expertise to maximize opportunities for the patient to accomplish their best possible health outcomes. This is a significant paradigm shift in interprofessional team-based care that simply must occur in our country.
The ambitious goal of the “Triple Aim” – (1) enhanced patient experience, (2) improved population health, and (3) reduced healthcare costs, now has become the “Quadruple Aim” (Annals of Family Med November/December 2014 vol. 12 no. 6) which also includes (4) improved health provider wellness. Widespread reports of provider burnout, particularly among physicians, now necessitates a team-based approach to healthcare that heretofore had been confined to closed health systems such as Veteran’s Administration centers and Kaiser Permanente institutions, just to name a few. Technology now allows improved communication among health providers so that all members may together construct a patient healthcare plan, provide meaningful contributions, and document their activities according to the direction of the primary provider. Collaborative Practice Agreements allow for proper oversight of the patient, while inserting accountability for patient safety and outcomes. Finally, the patient is transparently made aware of their provider network, and the contributions of each. Sharing healthcare responsibilities allows for population health principles to be applied, while maintaining the individual focus that each patient deserves.
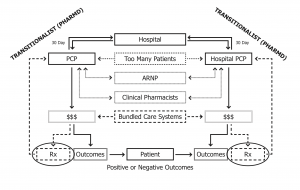
I have a fundamental plan to significantly transform the role of community pharmacists, and thus positively disrupt the healthcare system (see image). Patient-centered care can be achieved; it need not take another fifteen years for widespread implementation. Transformative utilization of pharmacist clinicians, with system-driven protocols, will significantly improve access to care for patients without increasing silos or breakdowns in provider communications. The Time is Now for Pharmacists to move from Behind the Counter and serve the public as valued medication specialists on team-based care units. Future postings will focus on a vision of the transformational role of pharmacist clinicians that will achieve the Quadruple Aim for people in all communities.