Until recently, scientists knew little about how important cells called fibroblasts might help protect the brain when a life-threatening bleeding stroke occurs.
But these cells may function like a plumber making an emergency house call, said Yao Yao, PhD, associate professor in Molecular Pharmacology and Physiology in the USF Health Morsani College of Medicine.
The analogy may help explain the healing power of fibroblasts, a type of cell that contributes to the formation of connective tissue.
Little has been known about fibroblasts in the brain until recently. But studying how they function there – and their healing power on the protective sheath called the blood-brain barrier (BBB) – could hold an important key to mitigating damage done by hemorrhagic strokes, for which there is currently no treatment, making them the deadliest kind of strokes.
“In the small vessels or capillaries of your brain, you normally don’t have any fibroblasts there because the vessels are tight – not leaky,” Dr. Yao said. “It’s like a home where all the plumbing system works perfectly. But when there’s a neurological disorder like a stroke, these small vessels become leaky and toxic blood components enter the brain. And we have found that fibroblasts travel from the large vessels to the small vessels, and repair a BBB injury.”
That, he explained, is the equivalent to fibroblasts serving as a plumber coming to fix broken pipes, with water suddenly pouring into the house.
“What we know so far is that the fibroblasts are functioning like the plumber,” Dr. Yao said. “They come. They repair damage. And then they leave.”
(Sadly, the plumber alluded to in the headline above, who achieved cartoon fame in the children’s TV show The Electric Company by telling a parrot, “It’s the plumber – I’ve come to fix the sink,” does not manage this kind of dignified departure.)
Dr. Yao and his team recently published their findings about fibroblasts (sans parrots) in the journal Cell Reports.
Some aspects of fibroblasts have been thoroughly studied, such as how these cells contribute to connective tissue in the skin. But for many years, scientists didn’t know that fibroblasts could be found within the brain or central nervous system. They were thought to exist only on the surface of the brain, in layers of the protective membrane called the meninges.
“But in 2018, there was a breakthrough with a report that said fibroblasts did exist in the brain, not just on the surface,” Dr. Yao said. “So the big question for us then was, ‘What do they do? What is their function?’ From skin studies, we knew that fibroblasts are known to repair injuries if, for instance, we cut ourselves. So in the brain, does the fibroblast do the same thing?”
This prompted Yao and his colleagues to conduct a thorough search of the existing literature about fibroblasts, which was limited to “four or five papers over the past 100 years,” he said.
Complicating the matter was that most existing studies utilized non-specific markers to identify the fibroblasts.
“Most fibroblast markers also label other cell populations,” Dr. Yao said. “When these markers are used, it is difficult to determine if fibroblasts or other cells are involved.”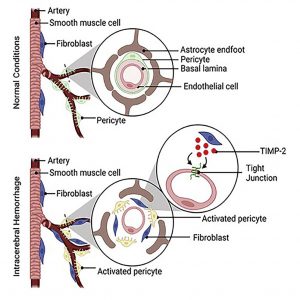
That led Dr. Yao’s group to study the 2018 paper, in which a marker unique to fibroblasts – known as collagen one-alpha-one (Col 1α1) was identified. That was the key step in starting their own work, leading in time to a significant discovery.
“We found out that fibroblasts do repair a very important structure called the blood-brain barrier – the area that separates blood from the central nervous system, the brain and spinal cord,” he said. “This is so important, because blood-brain barrier disruption is found in almost all neurological disorders – anything you can think of.”
Furthermore, they knew that after a brain injury or neurological disorder, it is critical to repair the disruption as quickly as possible. Tests were soon conducted on laboratory mice. Those mice deprived of fibroblasts experienced significant blood brain-barrier leakage and died within a week; those with fibroblasts recovered.
“So we had evidence,” he said. “The collagen one-alpha-one fibroblasts – in this population of mice – functioned to repair the BBB after hemorrhagic stroke.”
What comes next?
“Our goal is to fully understand the molecular mechanisms of fibroblast-mediated BBB repair, so that we can find a way to target fibroblasts to minimize neurological damage,” Yao said. “With this knowledge, we can signal fibroblasts to either come more quickly to repair BBB injury – mostly in the early phase of disease – or leave small vessels after the BBB is repaired to avoid fibrosis, which occurs mostly in the late phase of disease.”
Fibrosis can result when fibroblasts linger too long, causing a thickening or scarring of connective tissue. That led Dr. Yao back to his analogy.
“You wouldn’t want a plumber just to stay in your house when the job is done, either, just as you don’t want fibroblasts staying around when they complete their repair,” Dr. Yao said. He extends the comparison further. He and his team have learned that the fibroblasts accomplish their BBB repair by secreting a protein called TIMP2.
“Think of that as the plumber’s main tool for the job,” he said.
In addition to hoping to learn how to signal fibroblasts, Dr. Yao said he and his team will be looking into the future possibility of injecting TIMP2 directly to the injured brain, and circumventing the need for fibroblasts to deliver it.
Yao gives special credit to Lingling Xu, PhD, who played a leading role in the research and Cell Reports paper, and is now a post-doctoral researcher at Emory University. They worked together at the University of Georgia before Dr. Yao came to USF in 2021. “Our whole team will continue studying fibroblasts,” Dr. Xu said. “There’s still a long way to go to fully understand this cell.”
Meanwhile, they all know how high the stakes are in their research.
“When a hemorrhagic stroke happens, there’s not even one treatment for it, unlike ischemic strokes,” Dr. Yao said. “It is a leading cause of death. And hopefully our research will lead to saving many lives.”
— by Dave Scheiber for USF Health Communications
