USF Health researchers are studying how a little-known protein known as BIN1 may contribute to the formation of tangles in the brain that are a hallmark of Alzheimer’s disease, a degenerative brain condition that affects more than 6 million Americans today.
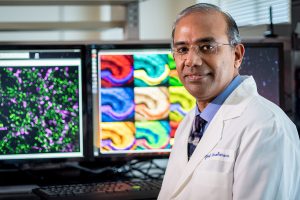
Their findings have been published in the peer-reviewed Brain: A Journal of Neurology. Leading the study was Gopal Thinakaran, PhD, CEO of the USF Health Byrd Alzheimer’s Center and Research Institute and professor of molecular medicine in the USF Health Morsani College of Medicine. Contributing to the report were Moorthi Ponnusamy, PhD, and other members of the Thinakaran Lab at the Byrd Institute.
The paper focuses on a protein called Bridging Integrator 1 – or BIN1 – a protein that is found in cells in the brain and other organs. Understanding BIN1 has been a challenge because it appears in different forms in brain cells, but breakthroughs could lead to improved therapies for people who develop Alzheimer’s as they age.
“Aging is the leading risk factor for Alzheimer’s disease,’’ Dr. Thinakaran said. “A comparison of small changes in the DNA of people worldwide with and without Alzheimer’s disease found up to 40% carry small changes in the BIN1 gene, and many of those are at a higher risk for developing the disease.’’
Until recently, other proteins, such as beta amyloid and tau, which contribute to the formation of plaques and tangles in the brain, have received more attention from researchers. But now scientists are turning to risk factors such as BIN1, believing understanding their function might offer targets for potential treatments.
BIN1 is the second-most prevalent genetic risk factor identified for late-onset Alzheimer’s disease. It encodes an adaptor protein that regulates certain functions in the brain, and evidence suggests BIN1 can alter the dynamics of cell membranes within the brain.
Thinakaran’s team looked at whether the presence of BIN1 inside the brain’s neurons favors the accumulation of tau, a toxic protein, in structures called tangles. Greater numbers of these tangles in the brain have been associated with memory loss and the death of brain cells.
The team found that laboratory mice without BIN1 in their neurons developed only milder degeneration in the regions of the brain essential for memory. Also, brain inflammation was reduced by the loss of BIN1, suggesting that BIN1 in neurons also influences nerve, or glial, cell activation during the development of Alzheimer’s disease.
“These findings mean that BIN1 in neurons promotes Alzheimer’s disease tau pathology, stimulates brain inflammation, and contributes to memory loss, thus identifying BIN1 as a possible drug target,’’ Dr. Thinakaran said.
The timing of the team’s work is critical: The number of Americans affected is expected to rise to 13 million by 2050 and cost the United States more than $1 trillion, according to the Alzheimer’s Association, a global voluntary health organization dedicated to care, support and research.
Alzheimer’s is a specific brain disease that progressively and irreversibly destroys memory and thinking skills. Eventually, Alzheimer’s disease takes away the ability to carry out even the simplest tasks.
The vast majority of people who develop Alzheimer’s dementia are age 65 or older. Experts believe this late-onset Alzheimer’s, like other common chronic diseases, develops as a result of multiple factors rather than a single cause. Although a handful of laboratories worldwide are studying how BIN1 is involved in the disease process, Thinakaran’s team is leading the research efforts to define how BIN1 acts as a risk for Alzheimer’s disease in the elderly.
Their work is funded by three major research grants totaling $7 million from the National Institute on Aging, which is part of the National Institutes of Health, along with grants from the Cure Alzheimer’s Fund and the Alzheimer’s Association.
In June, the USF Health group published a related study in the journal Molecular Neurodegeneraton, which described BIN1’s impact on glial cells, which are responsible for brain inflammation.
— Story by Kurt Loft for USF Health News
