For years Joyce Whidden suffered with heartburn and acid reflux. When an endoscopy revealed little more than mild redness, Whidden filled the prescription she was given for an acid reducer and resigned herself to living with the condition.
But things got worse for the Zellwood, FL resident.
“There was more regurgitation, more heartburn,” Whidden recalls. “I started sleeping on two pillows; eventually I migrated to the chair.”
A new doctor diagnosed the now 65-year-old Whidden with achalasia, a swallowing disorder that affects the ability of the esophagus to move food into the stomach. The only hope, he said, was a Heller myotomy, a complicated surgical procedure in which the muscles of the lower esophagus are cut to create an opening for food and liquids to pass.
Though desperate for relief, Whidden refused to consent to the procedure without more information – information her doctor was not able to provide.
“I wanted an explanation; this was a serious procedure,” she says. “I finally decided he wasn’t sure himself so I refused.”
But the condition was taking its toll. Whidden was losing her desire to eat, fearful of choking and increasingly aware of growing pressure and pain in her chest. More and more, liquids and solids were coming up into her mouth; none of the medications she was taking were working.
An answer in Tampa
Eventually Whidden was referred to the Joy McCann Culverhouse Center for Swallowing Disorders at USF Health. The nationally-renowned center had just come under the leadership of Joel E. Richter, MD, who joined USF in September from Temple University School of Medicine where he was chair of the Department of Medicine.
“I didn’t know I would be seeing Dr. Richter, but when I did, he put me at ease immediately,” Whidden recalls. “He explained to me in detail exactly how the condition went from minor to major. He explained why I felt this way, what could be done and what choices I had.”
And he told her about an endoscopic procedure that could prove to be the answer Whidden had sought for years. The outpatient procedure, called a pneumatic dilatation, involves inserting a sausage-shaped balloon into the narrowed ending of the esophagus and inflating it to create an opening for liquids and solid foods to pass into the stomach.
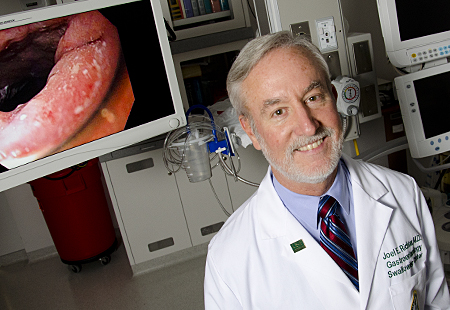
- Dr. Joel Richter, the new director of the USF Swallowing Disorders Center, told Whidden about an endoscopic procedure called pneumatic dilatation.
Over the course of his esteemed medical career, which includes 10 years as chair of the Department of Gastroenterology and Hepatology at the Cleveland Clinic Foundation, Dr. Richter has treated hundreds of patients with achalasia.
“A gastroenterologist in the community sees one or two cases a year; at USF, we see several in a week, ” he says. “We probably have the largest achalasia practice in the Southeast United States.”
Less than a week after Whidden’s visit to the USF center, Dr. Richter performed the pneumatic dilatation that would return her to a normal life.
“I had 100 percent confidence in him because of his experience and his explanation of why and when and how,” she says. “Within five days I was almost disease-free. All the heavy pressure and pain went away. I had the sensation of food moving down; I was absolutely thrilled.”
Achalasia is one of the complex swallowing and esophageal disorders Dr. Richter and his multi-specialty team treat at the stand-alone referral center. The center is part of the USF Division of Digestive Diseases and Nutrition which includes the university’s strong GI program.
Comprehensive treatment for complex disorders
Dr. Richter, the Hugh R. Culverhouse Chair for Esophagology at the USF College of Medicine, leads the division. He joined USF in the fall when H. Worth Boyce, MD, who built the university’s internally recognized swallowing program and led its clinical programs in digestive diseases, announced his retirement.
Today the division includes nine board-certified GI subspecialists and offers comprehensive care for patients with gastrointestinal disorders including gastrointestinal cancers, swallowing and esophageal diseases, irritable bowel syndrome, pancreatic biliary diseases, celiac disease and malabsorption, generalized GI motility disorders and women’s GI disorders.

The USF Health Division of Digestive Diseases and Nutrition’s multispecialty team offers comprehensive care for a wide array of gastrointestinal disorders.
Soohong Hong Chae, MD, joined the division in fall 2010 after completing a fellowship in gastroenterology at UCLA, Los Angeles. At USF, her practice is heavily focused on functional bowel diseases such as irritable bowel syndrome, small intestinal bacterial overgrowth, motility disorders such as pelvic floor dyssynergia, and inflammatory bowel disease. She has a strong interest in women’s gastrointestinal issues, particularly constipation.
Arthi Sanjeevi, MD, whose GI training was NIH-funded with a focus in GI motility disorders and neurogastroenterology, recently joined the division’s pancreatic biliary diseases group under the direction of Patrick Brady, MD. Her primary clinical interests focus on application of endoscopic ultrasound technology for improved diagnosis of gastrointestinal disorders and as an interventional tool in complicated pancreato-biliary disorders. In addition to routine endoscopy, Dr. Sanjeevi performs complex endoscopic procedures including endoscopic ultrasound, esophageal and enteral stent placements and deep enteroscopy.
Along with bringing new specialists to the program, Dr. Richter is introducing new technologies such as the Smart Pill, an ingestible capsule that uses sensor technology to measure motility (movement) from the stomach through the small bowel and into the colon. The pill, which collects information and sends it to a wireless receiver worn by the patient, is an alternative to gastric emptying scintigraphy which can take up to four hours. Breath tests that measure the presence of an ingested isotope in carbon dioxide, hydrogen or methane when a person exhales will also be available at the center to test for lactose intolerance and small bowel overgrowth motility.
Renewed focus on research
“We have a collegial group of physicians with a number of areas of interest and all doing research,” Dr. Richter says, adding that patient-oriented research is the greatest opportunity for advancing the program’s reputation.
“We have new treatments and new interventions because of USF research. The best clinical care is done in centers that are conducting cutting-edge, patient-oriented research.”
Dr. Richter says the best clinical care is done in centers, like USF’s, where leading-edge, patient-oriented research is a priority.
Dr. Richter’s career is steeped in the study of esophageal diseases. He has co-authored nearly 300 papers, 121 editorials and reviews, 11 books and 109 book chapters. In 1999, he developed the 48-hour Bravo pH test, a wireless pH test to measure acid coming up in the esophagus. Currently he is investigating new treatments for achalasia and eosinophilic esophagitis, a condition in which a certain type of white blood cells build up in the esophagus causing inflammation and injury.
His colleagues at the center, Dr. Boyce and David Estores, MD, are investigating restorative endoscopy, a novel therapy for head and neck cancer patients with severe radiation damage to the upper esophagus. USF is one of only a handful of GI centers in the nation conducting research in this area.
Nationally recognized swallowing center
At the swallowing center, Dr. Richter and Dr. Estores, treat patients with swallowing and other esophageal problems such as acid reflux, chest pain, regurgitation, food sticking, and solids and liquids not going down. The center’s dedicated multi-specialty team — the largest dedicated, full-time staff of any swallowing center in the United States — includes surgeons, an allergist, speech and rehabilitative therapists, and an advanced registered nurse practitioner. Once a week the team gets together to talk about clinical issues and research projects.
“It gives patients the appropriate assurance that they are coming to a center that is really focused on their problem – from the beginning of swallowing all the way down to the end of the esophagus,” Dr. Richter says, calling the center “one of the oldest and best endowed swallowing centers in the U.S.”
Building on a legacy of excellence
The Joy McCann Culverhouse Center for Swallowing Disorders was founded in 1987 following a generous gift from Joy Culverhouse. Dr. Boyce, the center’s founding director, grew the center to national prominence until his retirement in September 2011.
Dr. Richter is optimistic about continuing the center’s legacy of excellence. Since receiving his MD from the University of Texas Southwestern Medical School and completing an internship at the Naval Regional Medical Center in Philadelphia, PA, as well as a residency and fellowship at the National Naval Medical Center in Bethesda, MD, he has directed swallowing centers at the University of Alabama Medical Center, Cleveland Clinic and Temple University.
“The patients we see are scared to eat,” he says. They include patients like Whidden, who refers to the center as “where I found life.”
“I cannot begin to tell you the change in my life,” Whidden says, less than two months after undergoing the procedure at USF’s Morsani Center for Advanced Healthcare. “I cannot tell you how much better I feel – the joy I feel in my life. I will always sing Dr. Richter’s praises.”

A resource for community physicians
The gratitude comes from community physicians as well, physicians who refer difficult cases for evaluation and treatment. Recently, a patient from Arkansas was referred to the center for evaluation and treatment of lichen planus, a skin condition that can cause scar tissue in the lining of the esophagus, impairing a person’s ability to swallow. The referring gastroenterologist knew of the center’s reputation.
“As an academic referral center, we help demystify disease for practitioners in the community,” Dr. Richter says. “We are a place for consulting, diagnosis and treatment.” Typically patients return to their referring physician for follow-up care and continuing case management.
Untapped potential
As he settles into his new position at USF Health, Dr. Richter sees a program with tremendous untapped potential.
“My career has centered around building outstanding clinical care and research programs. This program will be second to none.”
Story by Ann Carney, and photos by Eric Younghans/USF Health Communications

